OCD is not a one-size-fits-all diagnosis, and is often greatly misunderstood. There are multiple severity levels of OCD and different obsessions and compulsions that you could be dealing with.
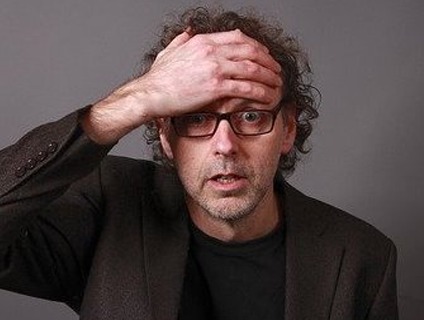
OCD feels like a losing battle against yourself; your brain is your own worst enemy. It’s a quest for control that is just out of reach. One of the most frustrating parts is you’re aware many of your obsessions aren’t practical. You fight it with logic, but it grows stronger. It absolutely will not listen to reason. It laughs at your evidence. It plays on your emotions. You want to beat it. You want to crush it – to simply kill it. Yet you struggle mightily. It’s exhausting and mentally draining to fight day in and day out.
There’s checking, washing, counting, tapping, fear of contamination, doubt, symmetry, arranging, and unacceptable thoughts. And one of the worst parts is feeling alone with this condition. It’s very difficult for someone without OCD to deeply relate – and you see it in their eyes when you explain yourself…So you stop explaining and start hiding. It becomes shameful. You know they won’t truly understand so why put yourself in a situation where you have to? You don’t go out as much, don’t live the life you want to. You know it’s irrational, but there’s a part of you that won’t be willing to take the risk of quitting the ritual, just in case this is the one time that it isn’t OCD – and there’s a very real threat. It’s the doom-and-gloom feeling that overcomes you if the compulsion is not allowed to manifest. And so it goes…
But you’re not alone. There are many others out there suffering in similar ways. You are understood here. Getting treatment is the first, and many times, scariest step in beating this and gaining back control. It’s why we go through a comprehensive assessment with you to create an individualized treatment plan allowing you to improve your life through YOUR own, unique journey.
Treatment of OCD at Khushi Mind Care includes :
A) Assessment :
1. Yale brown obsessive-compulsive scale(YBOCS)
2. Obsessive-compulsive inventory (OCI)
3. HAM-A(Hamilton rating scale for anxiety) Beck’s
4. Depression Inventory( BDI)
B) Medication:
SRIs often require higher daily doses in the treatment of OCD than depression and may take 8 to 12 weeks to start working, but some patients experience more rapid improvement.
C) Therapy/Counseling :
1. Cognitive-behavioral therapy (CBT) – methods to learn to identify and modify thought patterns accompanying obsessions and compulsions.
2. ERP- Exposure and Response Prevention is a specific type of CBT which aims to gradually desensitize one’s compulsive behaviors.
3. Psychodynamic Therapy – focused on revealing unconscious content of client’s psyche to alleviate psychic tension.
4. Social Rhythm Therapy – to develop normal sleep schedule and predicatble daily routines.
5. Family Therapy – psychoeducation of family regarding nature of illness, course and progression aiming to promote recovery